What is a Ganglion Cyst? A ganglion cyst is a...
Read MoreJoin us in exploring the multifaceted realm of the wrist. Discover its anatomy, from overuse to underlying health conditions, and learn about effective remedies and preventive strategies. Our articles cover the impact of repetitive tasks, ergonomic solutions, and therapeutic exercises to alleviate wrist pain.

What is a Ganglion Cyst? A ganglion cyst is a...
Read MoreCarpal tunnel syndrome: How to combat a costly problem Canadian...
Read MoreEndoscopic Procedure for Carpal Tunnel Syndrome: Faster Recovery Published on...
Read MoreWhat’s Really Causing Carpal Tunnel Syndrome? Published on Sanctuary Magazine...
Read MoreJoin us on a visual journey to unravel the complexities of wrist pain through our comprehensive video content. Dive into an array of informative videos dedicated to understanding the root causes of wrist discomfort, from injuries to chronic conditions. Explore step-by-step guides on exercises and stretches specifically designed to alleviate pain and improve wrist mobility. Our curated video collection offers expert insights, practical tips, and real-life demonstrations, providing an immersive learning experience.
Embark on an illuminating journey through our diverse array of articles, delving into the intricate world of the wrist. Explore a wealth of information encompassing various dimensions of wrist discomfort, from unraveling its root causes to navigating through tailored treatments and preventive strategies. Our articles delve into conditions like wrist arthritis, offering expert insights and practical advice. Uncover rehabilitative exercises, ergonomic suggestions, and lifestyle modifications aimed at enhancing wrist function and reducing discomfort.

Golfers & Tennis players in Bahamas benefit from Arthroscopy for assessing


Carpal tunnel syndrome: How to combat a costly problem Canadian HRReporter

Arthroscopic Resection of Dorsal Wrist Ganglia and Treatment of Recurrences Article
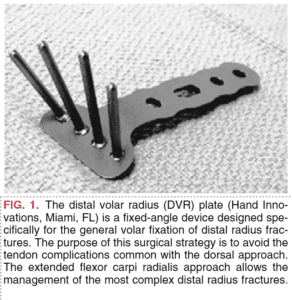
The Extended Flexor Carpi Radialis Approach: A New Perspective for the

Corrective osteotomy of dorsally malunited fractures of the distal radius via

Monday- Friday: 8:30AM- 5:00 PM
Saturday- Sunday: Closed