
Discover a wealth of information and insights about the fingers and their related conditions with us. Our resources cover a spectrum of topics, from the common causes of finger discomfort to specific conditions like injuries, swelling, and arthritis. Dive into articles exploring effective treatments, rehabilitation exercises, and preventive measures tailored to alleviate pain and enhance finger mobility. Whether you're seeking understanding about postural issues, sports-related injuries, or degenerative conditions, our comprehensive guides offer clarity and actionable advice. Our database contains multiple videos and articles that educate in finger centric topics, find more information below.
Join us on a visual journey to unravel the complexities of the finger through our comprehensive video content. Dive into an array of informative videos dedicated to understanding the root causes of finger discomfort, from injuries to chronic conditions. Explore step-by-step guides on exercises and stretches specifically designed to alleviate finger pain and improve finger mobility. Our curated video collection offers expert insights, practical tips, and real-life demonstrations, providing an immersive learning experience. Use the buttons below to navigate our database and find finger related content related to the topics of your interest.
Explore diverse topics encompassing the intricacies of finger discomfort, from understanding the root causes to practical strategies for relief. Uncover insights into recognizing early signs, implementing ergonomic adjustments, and discovering tailored exercises to alleviate discomfort. Our articles provide a roadmap to navigate through the complexities of finger pain, empowering you with actionable advice and expert perspectives. Whether you seek preventative measures or in-depth knowledge on specific finger conditions, our articles serve as a valuable resource to foster better finger health. If you continue to have doubts or questions regarding finger pain or any other orthopedic topic consider asking Dr. Badia a question using the Contact menu.


Jammed Finger May Be a Bigger Deal Than You Think Jammed

“Jammed Finger” Definition and Treatment Offers Tips For Finger Injuries in
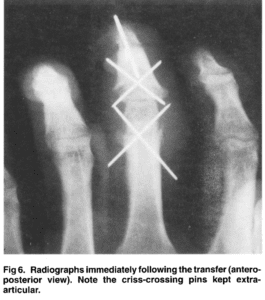
Distal interphalangeal joint to proximal interphalangeal joint homodigital island transfer Article

Percutaneous fixation of metacarpal fractures Article in Operative Techniques in Plastic

A simple fixation method for unstable bony mallet finger A simple

Monday- Friday: 8:30AM- 5:00 PM
Saturday- Sunday: Closed